
Gynecologic cancers affect thousands of women worldwide each year, and two of the most commonly discussed are ovarian cancer and endometrial cancer. While both arise in the female reproductive system, they differ significantly in origin, presentation, diagnosis, and treatment.
At MACS Clinic,, we prioritize patient education to help individuals make informed health decisions. According to Dr. Sandeep Nayak, a surgical oncologist in Bangalore, “Early diagnosis begins with awareness. Understanding how ovarian and endometrial cancers differ can lead to timely interventions and potentially better outcomes
What Is Ovarian Cancer?
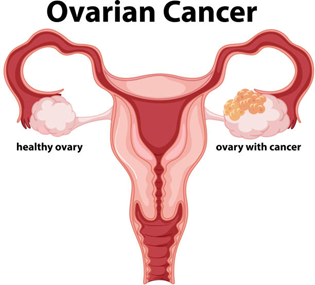
Ovarian cancer originates in the ovaries, the female reproductive glands responsible for producing eggs and hormones like estrogen and progesterone. It is often referred to as a “silent” cancer because symptoms may be vague or go unnoticed in the early stages.
There are several types of ovarian cancer, with epithelial ovarian cancer being the most common, accounting for about 90% of all cases. Others include germ cell tumors and stromal tumors, which are less frequent but typically affect younger women.
Common early symptoms of ovarian cancer include:
- Persistent bloating
- Pelvic or abdominal pain
- Early satiety (feeling full quickly)
- Frequent urge to urinate
The lack of specific early warning signs often leads to late-stage diagnosis. Dr. Sandeep Nayak notes, “Many patients diagnosed with ovarian cancer report subtle symptoms that were initially dismissed. This makes awareness and regular evaluations incredibly important.”
What Is Endometrial Cancer?
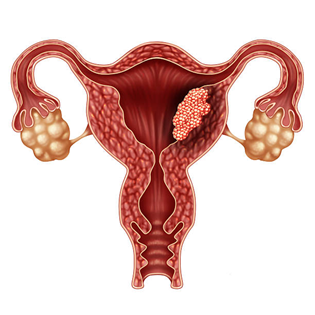
Endometrial cancer begins in the lining of the uterus, called the endometrium. It generally affects postmenopausal women, although younger women can also be diagnosed.
There are two main categories:
- Type I (estrogen-dependent): Slower growing and more common.
- Type II: More aggressive and not hormone-related.
Unlike ovarian cancer, endometrial cancer often produces noticeable symptoms early on, which aids in prompt diagnosis.
Signs of endometrial cancer include:
- Vaginal bleeding after menopause
- Heavy or prolonged periods
- Pelvic discomfort
- Watery or blood-tinged vaginal discharge
Due to its early presentation, the survival rate for endometrial cancer is generally higher compared to ovarian cancer.
Key Differences Between Ovarian and Endometrial Cancer
When comparing ovarian cancer vs. endometrial cancer, the contrasts are significant across several aspects:
|
Feature |
Ovarian Cancer |
Endometrial Cancer |
|
Origin |
Ovaries |
Uterine lining |
|
Common Age Group |
50–65 years |
Postmenopausal (over 55) |
|
Early Symptoms |
Often absent or vague |
Noticeable (e.g., vaginal bleeding) |
|
Diagnosis Stage |
Frequently late-stage |
Often early-stage |
|
Prognosis |
Generally guarded |
Generally favorable |
|
Detection |
Requires imaging and tumor markers |
Often via biopsy |
Symptoms Comparison

Recognizing early symptoms is crucial in both cancers. However, the endometrial cancer vs ovarian cancer symptoms show clear contrasts:
Ovarian Cancer Symptoms:
- Abdominal bloating or swelling
- Difficulty eating or feeling full quickly
- Frequent urination
- Unexplained fatigue
Endometrial Cancer Symptoms:
- Vaginal bleeding after menopause
- Bleeding between periods
- Pelvic or lower abdominal pain
- Watery or blood-tinged vaginal discharge
Ovarian cancer symptoms are often gastrointestinal in nature and easily mistaken for digestive issues. In contrast, endometrial cancer tends to produce direct gynecologic signs, such as abnormal uterine bleeding—making it easier to detect early.
Causes and Risk Factors
Both cancers are influenced by hormonal, genetic, and lifestyle factors, but they differ in key risk contributors.
Ovarian Cancer Risk Factors:
- Family history of ovarian or breast cancer
- BRCA1 or BRCA2 gene mutations
- Increasing age
- Infertility or never having been pregnant
- Hormone replacement therapy
Endometrial Cancer Causes:
- Obesity (increased estrogen exposure)
- Early menstruation or late menopause
- Diabetes and hypertension
- Tamoxifen use
- Polycystic ovarian syndrome (PCOS)
“BRCA genes play a significant role in ovarian cancer but can also be relevant to endometrial cancers in certain genetic syndromes,” explains Dr. Nayak.
Diagnosis Methods

Ovarian Cancer Diagnosis:
- Pelvic ultrasound
- CA-125 blood test (tumor marker)
- CT scan or MRI
- Surgical biopsy (often required for definitive diagnosis)
Endometrial Cancer Diagnosis:
- Transvaginal ultrasound
- Endometrial biopsy
- Hysteroscopy
- Dilation and curettage (D&C)
Because ovarian cancer is often hidden deep within the pelvic cavity, it may require more advanced imaging and surgical evaluation. In contrast, signs of endometrial cancer can be detected with relatively straightforward outpatient procedures.
Treatment Options
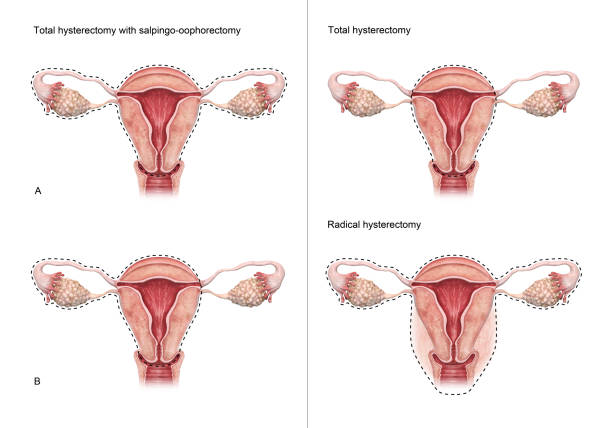
Treatment depends on the cancer type, stage, and the patient’s overall health.
Ovarian Cancer Treatment:
- Surgery (total hysterectomy with removal of ovaries and fallopian tubes)
- Chemotherapy
- Targeted therapy
- Occasionally, radiation therapy
Endometrial Cancer Treatment:
- Surgery (hysterectomy)
- Radiation therapy
- Hormonal therapy (especially in early-stage Type I cancers)
- Chemotherapy for aggressive or advanced cases
minimally invasive surgical techniques, including robotic-assisted surgery, may be considered to reduce recovery time and potentially improve outcomes, depending on individual patient factors.
Prognosis and Survival Rates
Ovarian Cancer:
- 5-year survival (early-stage): Approximately 90%
- 5-year survival (late-stage): 30–40%
Endometrial Cancer:
- 5-year survival (early-stage): Around 95%
- 5-year survival (advanced stage): 17–30%
Ovarian cancer has a more guarded prognosis due to later detection. However, advances in targeted therapy have significantly improved outcomes in recent years.
Preventive Measures and Screening
While no absolute prevention exists, you can reduce risk.
Ovarian Cancer Prevention:
- Genetic testing if family history exists
- Oral contraceptives (may lower risk)
- Prophylactic oophorectomy for BRCA-positive individuals
Endometrial Cancer Prevention:
- Maintaining a healthy weight
- Managing hormonal imbalances
- Treating underlying conditions like PCOS and diabetes
- Avoiding unopposed estrogen therapy
No routine screening tests exist for either, but awareness of symptoms is crucial.
When to See a Doctor

While no absolute prevention exists, you can reduce risk.
Ovarian Cancer Prevention:
- Genetic testing if family history exists
- Oral contraceptives (may lower risk)
- Prophylactic oophorectomy for BRCA-positive individuals
Endometrial Cancer Prevention:
- Maintaining a healthy weight
- Managing hormonal imbalances
- Treating underlying conditions like PCOS and diabetes
- Avoiding unopposed estrogen therapy
No routine screening tests exist for either, but awareness of symptoms is crucial.
Conclusion
Understanding the difference between ovarian and endometrial cancer equips women with knowledge that can save lives. While both are gynecologic cancers, they differ vastly in origin, symptoms, diagnosis, and treatment. Prompt medical evaluation ensures the best possible outcomes.
Whether you are concerned about symptoms, exploring prevention, or seeking a second opinion, consult a qualified healthcare professional. Individual results may vary.
Frequently Asked Questions
Can endometriosis cause cancer?
Is ovarian cancer curable?
Is endometrial cancer the same as ovarian cancer?
Is ovarian cancer dangerous?
Can endometrial cancer turn into ovarian cancer?
Are BRCA genes related to both cancers?
Reference
https://www.healthline.com/health/ovarian-cancer/endometrial-cancer-vs-ovarian-cancer#outlook
https://www.americanoncology.com/blogs/how-do-endometrial-cancer-and-ovarian-cancer-differ
Disclaimer: This information is for educational purposes only and is not a substitute for professional medical advice. Individual results may vary. Please consult a qualified doctor for personalized recommendations.
