This page covers the management of Medullary Thyroid Cancer (MTC), a rare form of thyroid malignancy that often requires specialized care. It outlines the latest diagnostic tools, genetic screening protocols, and advanced surgical treatments available for MTC. The information is developed with insights from MACS Clinic and Dr. Sandeep Nayak, a globally recognized surgical oncologist based in Bangalore, India. Dr. Nayak is the pioneer of the RABIT technique—a robotic thyroidectomy approach that offers a scarless and precision-driven alternative to conventional surgery, particularly valuable in complex cases like MTC.
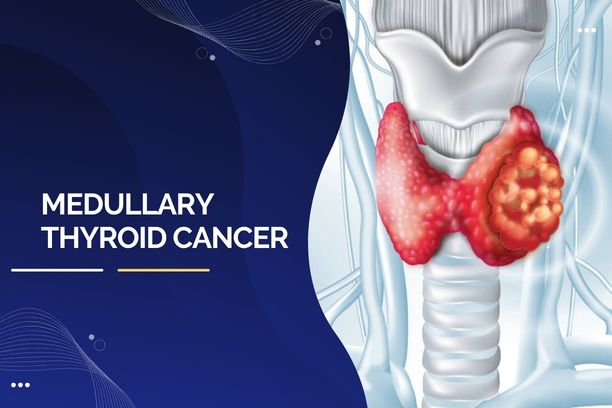
What Is Medullary Thyroid Cancer?
Medullary thyroid cancer accounts for about 3–4% of all thyroid cancer cases, yet it remains a major clinical focus due to its unique behavior and potential to be hereditary. It originates from C cells, which are responsible for producing calcitonin, a hormone involved in calcium regulation.
There are two major types of MTC:
- Sporadic MTC: Occurs in individuals without a family history and constitutes approximately 75% of cases.
- Hereditary MTC: Makes up about 25% and is linked to RET gene mutations, often as part of MEN 2 syndrome.
Although MTC tends to be more aggressive than differentiated thyroid cancers, advances in early detection, genetic testing, and surgical precision have vastly improved prognoses.
“Medullary thyroid cancer requires a multidisciplinary, gene-guided approach. The key is precise diagnosis, followed by meticulous surgical intervention—ideally before the disease spreads.”— Dr. Sandeep Nayak, Surgical Oncologist, Bangalore.
Let’s look at what increases the risk of developing medullary thyroid cancer.
Causes and Risk Factors of MTC
Understanding the root causes can guide both treatment and prevention.
Primary Causes:
- Genetic Mutation (RET gene): A majority of hereditary MTC cases stem from mutations in the RET proto-oncogene.
- MEN 2 Syndrome: This includes MEN 2A and MEN 2B, conditions associated with multiple endocrine tumors, including MTC.
Other Risk Factors:
- Family history of MTC or MEN 2
- Radiation exposure (though less relevant in MTC compared to other thyroid cancers)
- Age and gender: Sporadic MTC commonly affects individuals in their 40s to 60s and is slightly more common in females.
These factors make genetic testing for thyroid cancer vital, especially in families with a history of endocrine tumors.
Let’s now examine the warning signs.
Common Symptoms of Medullary Thyroid Cancer

Medullary thyroid cancer symptoms may appear subtly at first but can become more pronounced as the tumor grows.
Symptoms Include:
- A painless lump or swelling in the neck
- Hoarseness or changes in voice
- Difficulty swallowing
- Swollen lymph nodes in the neck
- Diarrhea (due to hormone production by the tumor)
- Facial flushing or redness
Because these symptoms can mimic other benign conditions, they are often overlooked. Hence, timely assessment is crucial.
How Is Medullary Thyroid Cancer Diagnosed?

Diagnosing MTC involves a combination of imaging, lab tests, and sometimes genetic analysis. Here’s how it works:
Blood Tests:
- Calcitonin: High levels are a key indicator of MTC.
- CEA (Carcinoembryonic Antigen): Another tumor marker used for prognosis and monitoring.
Imaging:
- Ultrasound of the neck: Identifies thyroid nodules and enlarged lymph nodes.
- CT or MRI scans: Used when there’s suspicion of spread beyond the neck.
- PET scans: Occasionally used to locate metastases if calcitonin remains high after surgery.
Fine-Needle Aspiration (FNA) Biopsy:
- A small sample is taken from the thyroid nodule using a thin needle.
- If calcitonin is measured in the biopsy fluid, it can confirm MTC even before surgery.
Genetic Testing:
If MTC is confirmed, RET gene testing is recommended for the patient and close family members to assess hereditary risk.
Staging and Classification of MTC
Once MTC is diagnosed, staging helps determine how far it has progressed.
- Stage I: Tumor is small and confined to the thyroid.
- Stage II: Tumor has grown larger but hasn’t spread outside the thyroid.
- Stage III: Cancer has spread to nearby lymph nodes in the neck.
- Stage IV: Cancer has spread to distant parts of the bodylike the liver, lungs, or bones.
The staging system helps doctors choose the most effective treatment and estimate prognosis. Early stages usually respond very well to surgery, while later stages may require targeted treatments or close follow-up.
Let’s look at how this condition is treated.
Treatment Options for Medullary Thyroid Cancer
The mainstay of medullary thyroid cancer treatment is surgery, but depending on the stage, other options may also be needed.

Surgical Management:
- Total Thyroidectomy: Removal of the entire thyroid gland is necessary to prevent recurrence.
- Neck Lymph Node Dissection: If cancer has spread to nearby nodes, these are also removed during surgery.
At advanced centers like MACS Clinic, the RABIT technique (Robotic-Assisted Breast-axillo Insufflation Thyroidectomy) allows for precise, minimally invasive surgery with no visible scar on the neck.
Medical Treatments:
- Targeted Therapy: In advanced or metastatic MTC, medications such as vandetanib or cabozantinib block the signals that help cancer grow.
- Radiotherapy: Rarely used but may help in palliative cases where surgery isn’t possible.
Radioactive iodine, commonly used in other thyroid cancers, is not effective in MTC due to the nature of C cells.
What happens after the initial treatment?
Post-Treatment Monitoring and Follow-Up Care
Ongoing monitoring is essential to detect recurrence early and manage long-term health.
Regular follow-up includes:
- Calcitonin and CEA testing: If levels rise, it may indicate recurrence or residual disease.
- Neck ultrasound: To check for new nodules or lymph node changes.
- Imaging Scans: CT or PET scans may be necessary if recurrence is suspected.
Patients may require lifelong follow-up due to the risk of delayed recurrence, particularly in hereditary cases.
Let’s understand why catching it early makes all the difference.
Why Early Diagnosis Matters in MTC
Early detection offers the highest chance of curative treatment and prevents metastasis.
Benefits include:
- Higher surgical success rates
- Avoidance of distant organ involvement
- Improved survival outcomes
In hereditary cases, prophylactic thyroidectomy in RET-positive individuals—especially children—can prevent cancer altogether.
Who needs it?
Genetic Counseling and Family Screening
Anyone diagnosed with MTC, especially under age 50, or with a family history of thyroid or endocrine tumors, should consider genetic counseling.

Key Elements:
- Genetic Testing: RET mutation screening in immediate relatives.
- Counseling: To understand inheritance patterns and options.
- Preventive Surgery: Prophylactic thyroidectomyin children with MEN 2 mutations is often recommended.
Such proactive steps can truly be life-saving for entire families.
So, what does life look like after treatment? Let’s take a closer look.
Living with Medullary Thyroid Cancer
Anyone diagnosed with MTC, especially under age 50, or with a family history of thyroid or endocrine tumors, should consider genetic counseling.

While MTC presents unique challenges, many patients lead fulfilling lives with proper care.
Tips for long-term well-being:
- Stay consistent with follow-up visits
- Take thyroid hormone replacement as prescribed
- Talk to a counselor or join a support group to manage emotional stress
Frequently Asked Questions
What makes medullary thyroid cancer different from other thyroid cancers?
It originates from C cells, not follicular cells, and often has a genetic cause involving the RET gene. It also doesn’t respond to radioactive iodine.
Is medullary thyroid cancer hereditary?
Yes, about 25% of cases are hereditary, linked to MEN 2 syndrome and RET gene mutation.
What role does calcitonin play in diagnosing MTC?
Elevated calcitonin is a hallmark of MTC and helps in both diagnosis and post-treatment monitoring.
Is surgery always required for MTC?
Yes, surgery is the primary treatment and is essential to remove the tumor and reduce the risk of spread.
Can Medullary Thyroid Cancer spread to other organs?
Yes, MTC can metastasize to lymph nodes, liver, lungs, and bones if not treated early.
How often should calcitonin levels be monitored after treatment?
Initially, every 3–6 months, and later annually, depending on patient response and disease statu
Reference links:
https://www.healthline.com/health/papillary-vs-follicular-thyroid-cancer
https://pmc.ncbi.nlm.nih.gov/articles/PMC4383844/
Disclaimer: This page is for informational purposes only. Individual results may vary. Consult a qualified doctor for personalized advice.