Thyroid cancer, the most prevalent endocrine malignancy, has been witnessing a steady rise globally. In India, the incidence of thyroid cancer is increasing, with projections indicating a continued upward trend. Among the various types, papillary and follicular thyroid cancers are the most common, collectively referred to as differentiated thyroid cancers. Understanding the distinctions between Papillary vs. Follicular Thyroid Cancer is crucial for effective diagnosis and treatment.
Dr. Sandeep Nayak, a surgical oncologist in India, emphasizes, “While both papillary and follicular thyroid cancers are generally treatable, their management strategies differ due to variations in behavior and spread patterns.” He has experience in minimally invasive and robotic thyroid surgeries, which may offer benefits such as smaller incisions and faster recovery for some patients.
At MACS Clinic, Bangalore, Dr. Nayak and his team offer advanced surgical techniques, including the RABIT procedure, which is designed to minimize visible scarring and provide precise treatment options for thyroid cancer patients. They focus on individualized care to support the best possible outcomes for each patient.
First, let’s get a clear picture of the basics before diving deeper.
Understanding Thyroid Cancer Types: A Quick Overview
The most common type, accounting for approximately 80% of thyroid cancer cases. It typically grows slowly and often spreads to lymph nodes in the neck.
The second most common type, representing about 10-15% of cases. It tends to spread through the bloodstream to distant organs like the lungs and bones.
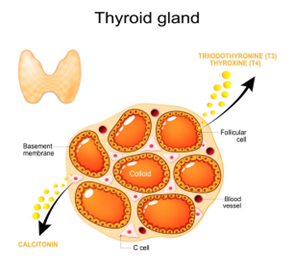
Both types are considered differentiated thyroid cancers, originating from follicular cells, but they differ in their histological features and patterns of spread.
Papillary vs. Follicular Thyroid Cancer: Key Differences
| Feature |
Papillary Thyroid Cancer (PTC)
|
Follicular Thyroid Cancer (FTC) |
| Prevalence | Most common (≈80%) |
Second most common (≈10-15%)
|
| Age Group Affected | Common in younger individuals (30-50 years) |
More prevalent in older individuals (40-60 years)
|
| Gender Predilection |
More common in women
|
Slightly more common in women |
| Histology | Papillary structures, nuclear features |
Follicular patterns, capsular/vascular invasion
|
| Spread Pattern | Lymphatic spread to cervical lymph nodes |
Hematogenous spread to lungs and bones
|
| Prognosis | Excellent with high survival rates |
Good, slightly less favorable than PTC
|
| Treatment Approach | Often involves total thyroidectomy + radioactive iodine |
Similar, varies based on spread
|
Not sure what type of thyroid cancer you have? Consult a qualified cancer care professional for personalized advice.
Curious about what could lead to thyroid cancer? Let’s discuss the primary triggers and risk factors.
What Causes These Thyroid Cancers?

Exposure to Radiation: Radiation exposure, particularly in early childhood, increases the risk for both PTC and FTC.
- Iodine Deficiency: FTC is more frequently linked with iodine-deficient areas, highlighting the need for sufficient iodine.
- Genetic Factors: Specific gene mutations, for example, BRAF in PTC and RAS in FTC, contribute to the development of these cancers.
- Family History: A family history of thyroid cancer or associated syndromes increases risk.
- Hormonal Factors: Estrogen is suspected to have some role, with these cancers being more frequent in women.
- Environmental Toxins: Exposure to specific chemicals over the long term may also increase risk, although evidence is still emerging.
Symptoms of Papillary and Follicular Thyroid Cancer

Swelling in the Neck or Lump: Frequently the initial apparent sign, typically painless and midline at the lower front of the neck.
- Hoarseness or Change in Voice: Particularly if the tumor compresses or involves the vocal cords.
- Trouble Swallowing: An enlarging nodule or tumor can put pressure on the esophagus, causing difficulty in swallowing.
- Breathing Difficulty: Compression of the trachea can result in shortness of breath.
- Chronic Neck Pain: Particularly if it spreads to the jaw or ears.
- Enlarged Lymph Nodes: Most typical in papillary thyroid cancer, these can present as firm, swollen masses in the neck.
How Are They Diagnosed?
This is how the diagnosis process typically works:
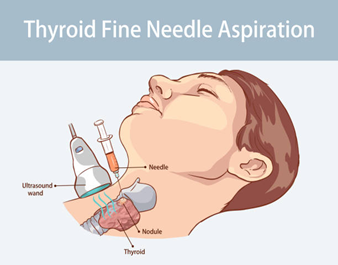
- Physical Examination:
A medical professional inspects for lumps, asymmetry, or swelling of lymph nodes in the neck.

- Ultrasound Imaging:
High-resolution thyroid ultrasound provides detailed visuals of the gland, helping assess size, structure, and suspicious features of nodules.

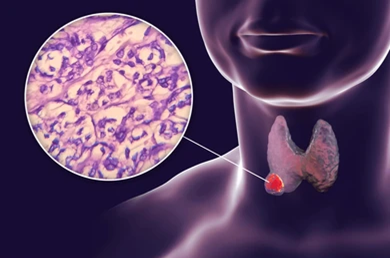
- Fine-Needle Aspiration Biopsy (FNAB):
A thin needle extracts cells from a thyroid nodule for laboratory examination under a microscope.
- Thyroid Function Tests:
Blood tests to measure T3, T4, and TSH levels, identifying whether the thyroid is underactive, overactive, or functioning normally.
- Thyroid Function Tests:
Blood tests to measure T3, T4, and TSH levels, identifying whether the thyroid is underactive, overactive, or functioning normally.
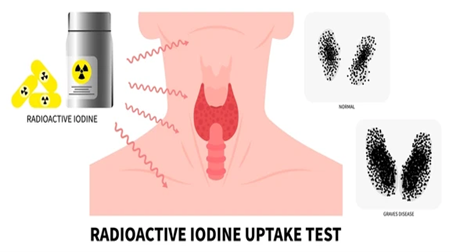
- Radioactive Iodine Uptake Scan:
Evaluates whether nodules absorb iodine, distinguishing between “hot” (usually non-cancerous) and “cold” (potentially cancerous) nodules.
- CT or MRI Scans:
Advanced imaging used when there’s suspicion of cancer spread beyond the thyroid or into nearby structures.
Treatment Options
This is how the diagnosis process typically works:
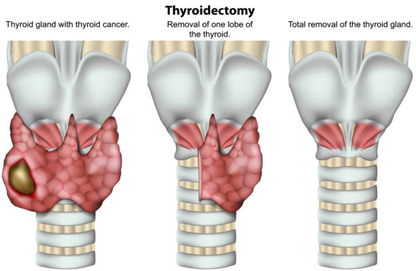
- Surgery:
The initial treatment generally includes the removal of some or the entire thyroid gland (lobectomy or total thyroidectomy). The selection is based on tumor size, extent, and general health.
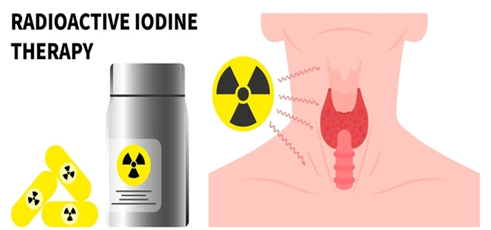
- Radioactive Iodine Therapy (RAI):
RAI after surgery is used to destroy any remaining thyroid tissue or cancer cells, particularly in papillary thyroid cancer.
- Thyroid Hormone Replacement Therapy:
Patients are usually prescribed lifelong levothyroxine to replace thyroid hormone and suppress TSH, which may help reduce the risk of cancer recurrence.

- External Beam Radiation Therapy:
Applied in exceptional instances if RAI fails or for cancers that are inoperable and have spread.

- Targeted Therapy:
Medications such as tyrosine kinase inhibitors are applied for advanced or RAI-resistant cancer in order to inhibit certain cancer-promoting proteins.
- Ongoing Monitoring:
Routine follow-up entails physical examination, blood work (thyroglobulin levels), and imaging to identify any recurrence early.
Conclusion
Understanding the differences between papillary vs. follicular thyroid cancers is vital for accurate diagnosis and effective treatment. While both types have high treatment success rates, their management strategies differ. Consulting with experienced specialists ensures access to advanced surgical techniques and personalized care, enhancing patient outcomes.
Frequently Asked Questions
Which thyroid cancer is more dangerous—papillary or follicular?
Though both have good survival rates, follicular thyroid cancer can be more aggressive because it may spread to distant organs.
Can thyroid cancer return after treatment?
Can a person live a normal life after thyroid cancer treatment?
Are there lifestyle changes recommended after treatment?
How often should follow-up visits be scheduled?
Which is worse, papillary or follicular thyroid cancer?
What’s the difference in papillary vs follicular thyroid cancer histology?
How does papillary vs follicular thyroid cancer spread differ?
Reference links:
https://www.healthline.com/health/papillary-vs-follicular-thyroid-cancer
https://pmc.ncbi.nlm.nih.gov/articles/PMC4383844/
Disclaimer: This page is for informational purposes only. Individual results may vary. Consult a qualified doctor for personalized advice.